Ankylosing Spondylitis
What is ankylosing spondylitis?
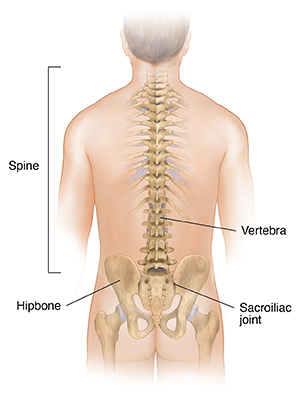
Ankylosing spondylitis (AS) is a type of arthritis that causes inflammation in certain parts of the spine. Ankylosing means stiff or rigid. Spondyl means spine. Itis refers to inflammation. The disease causes inflammation of the spine and large joints, resulting in stiffness and pain. The disease may damage the joint between the spine and the hipbone. This is called the sacroiliac joint. It may also cause bony bridges to form between vertebrae in the spine, fusing those bones. Bones in the chest may also fuse.
What causes ankylosing spondylitis?
The exact cause of AS is unknown. But researchers think that genetics play a role. A gene called HLA-B27 is found in most white Americans who have AS. But this gene is found in only 50% of African Americans who have AS. There are also some people with the HLA-B27 gene that don't develop AS. Less than 5% of people with the HLA-B27 gene have AS.
Who is at risk for ankylosing spondylitis?
AS is more common among people ages 17 to 35. It can happen in children and older adults, as well. The disease affects more young men than women. It tends to run in families.
What are the symptoms of ankylosing spondylitis?
Symptoms of AS tend to come and go over time. Symptoms can occur a bit differently in each person. The symptoms may include:
-
Back pain, usually most severe at night during rest
-
Early morning stiffness
-
Stooped posture in response to back pain (bending forward tends to relieve the pain)
-
Straight and stiff spine
-
Inability to take a deep breath, if the joints between the ribs and spine are affected
-
Appetite loss
-
Weight loss
-
Fatigue
-
Fever
-
Anemia
-
Joint pain
-
Mild eye inflammation
-
Organ damage, such as to the heart, lungs, and eyes
-
Skin rashes
-
Digestive illness (such as Crohn's or ulcerative colitis)
Many of these symptoms may be caused by other health problems. Make sure to see your healthcare provider for a diagnosis.
How is ankylosing spondylitis diagnosed?
Diagnosis starts with a health history and physical exam. You may also need tests, such as:
-
X-ray. This test uses a small amount of radiation to create images of internal tissues, bones, and organs onto film.
-
Erythrocyte sedimentation rate (ESR or sed rate). This test looks at how quickly red blood cells fall to the bottom of a test tube. When swelling and inflammation are present, the blood's proteins clump together and become heavier than normal. They fall and settle faster at the bottom of the test tube. The faster the blood cells fall, the more severe the inflammation. Up to 7 in 10 people with AS have a high ESR.
-
Genetic testing. Genetic testing is done to find if a person carries a copy of an altered gene for a disease. The gene HLA-B27 is found in more than 19 in 20 people with AS.
How is ankylosing spondylitis treated?
Treatment will depend on your symptoms, your age, and your general health. It will also depend on how severe the condition is. The goal of treatment is to ease pain and stiffness, prevent deformities, and maintain as normal a lifestyle as possible. Treatment may include:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs), to ease pain and inflammation
-
Tumor-necrosis-factor blockers (biologic medicines), to ease inflammation and swelling
-
Interleukin-17A (IL-17A) inhibitors, to ease inflammation and swelling
-
Disease-modifying anti-rheumatic medicines (DMARDs), such as sulfasalazine, to ease inflammation and control AS
-
Short-term use of corticosteroids, to ease inflammation
-
Short-term use of muscle relaxants and pain relievers, to ease severe pain and muscle spasms
-
Surgery to replace a joint, place rods in the spine, or remove parts of the thickened and hardened bone
-
Maintaining of proper posture
-
Regular exercise, including exercises that strengthen back muscles
Talk with your healthcare provider about the risks, benefits, and possible side effects of all medicines.
What are the possible complications of ankylosing spondylitis?
Over time, a forward curve of the spine can develop in people with AS. People with AS are at great risk of thinning of the bones (osteoporosis). This can result in spinal fractures. In more advanced cases, inflammation leads to new bone formation in the spine. This causes parts of the spine to fuse together, resulting in immobility. AS can also lead to psoriasis, and inflammation of the eye, aortic valve, and intestinal tract.
Living with ankylosing spondylitis
There is no cure for AS, so it is important to work on a treatment plan with your healthcare provider. Work on lifestyle changes that can improve your quality of life. Stay active and keep up with exercise to reduce pain. A physical therapist can help you design an exercise plan and help you keep a good posture.
When should I call my healthcare provider?
If your symptoms get worse or you have new symptoms, let your healthcare provider know right away.
Key points about ankylosing spondylitis
-
Ankylosing spondylitis is a type of arthritis that causes inflammation in certain parts of the spine.
-
A gene may be part of the cause of AS. But an exact cause is unknown.
-
Symptoms of AS include back pain, early morning stiffness, and a stooped posture.
-
AS can cause other symptoms such as appetite loss, weight loss, fatigue, fever, anemia, eye inflammation, and digestive illness.
-
The goal of treatment for AS is to ease pain and stiffness, prevent deformities, and maintain as normal a lifestyle as possible.
-
Staying active is important in the management of AS.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are and when they should be reported.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is advised and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions.